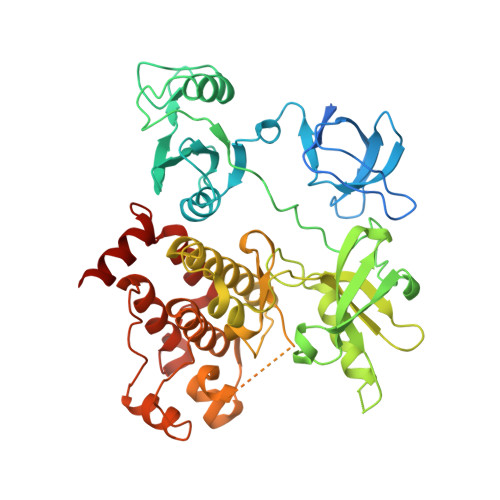
The allosteric inhibitor ABL001 enables dual targeting of BCR-ABL1.
Wylie, A.A., Schoepfer, J., Jahnke, W., Cowan-Jacob, S.W., Loo, A., Furet, P., Marzinzik, A.L., Pelle, X., Donovan, J., Zhu, W., Buonamici, S., Hassan, A.Q., Lombardo, F., Iyer, V., Palmer, M., Berellini, G., Dodd, S., Thohan, S., Bitter, H., Branford, S., Ross, D.M., Hughes, T.P., Petruzzelli, L., Vanasse, K.G., Warmuth, M., Hofmann, F., Keen, N.J., Sellers, W.R.(2017) Nature 543: 733-737
- PubMed: 28329763
- DOI: https://doi.org/10.1038/nature21702
- Primary Citation of Related Structures:
5MO4 - PubMed Abstract:
Chronic myeloid leukaemia (CML) is driven by the activity of the BCR-ABL1 fusion oncoprotein. ABL1 kinase inhibitors have improved the clinical outcomes for patients with CML, with over 80% of patients treated with imatinib surviving for more than 10 years. Second-generation ABL1 kinase inhibitors induce more potent molecular responses in both previously untreated and imatinib-resistant patients with CML. Studies in patients with chronic-phase CML have shown that around 50% of patients who achieve and maintain undetectable BCR-ABL1 transcript levels for at least 2 years remain disease-free after the withdrawal of treatment. Here we characterize ABL001 (asciminib), a potent and selective allosteric ABL1 inhibitor that is undergoing clinical development testing in patients with CML and Philadelphia chromosome-positive (Ph + ) acute lymphoblastic leukaemia. In contrast to catalytic-site ABL1 kinase inhibitors, ABL001 binds to the myristoyl pocket of ABL1 and induces the formation of an inactive kinase conformation. ABL001 and second-generation catalytic inhibitors have similar cellular potencies but distinct patterns of resistance mutations, with genetic barcoding studies revealing pre-existing clonal populations with no shared resistance between ABL001 and the catalytic inhibitor nilotinib. Consistent with this profile, acquired resistance was observed with single-agent therapy in mice; however, the combination of ABL001 and nilotinib led to complete disease control and eradicated CML xenograft tumours without recurrence after the cessation of treatment.
- Novartis Institutes for BioMedical Research, Cambridge, Massachusetts 02139, USA.
Organizational Affiliation: